3 Historical Background
The CRAG Working Group on “IT to Support Shared Care in Diabetes” in its diabetes dataset recommended a 10-point mutually exclusive grading nomenclature, with the presence or absence of maculopathy assessed separately. The CRAG dataset did not include definitions of each level, but referred to the Royal College of Ophthalmologists 1997 guidelines for diabetic retinopathy, for the precise definition of the grades. These are based on a clinical modification of the Early Treatment of Diabetic Retinopathy Study (ETDRS) retinopathy severity scale. The CRAG dataset also did not specify what screening technology should be used.
In the CRAG dataset the term background diabetic retinopathy (BDR) was used in place of non-proliferative diabetic retinopathy (NPDR) as used in the Royal College Guidelines. Four quadrants of the retina, centred on the disc, had to be available to permit complete assessment by this methodology. This meant that a minimum of two photographic fields were required (e.g. EURODIAB photographic protocol).
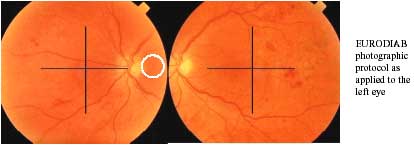
However, more recent evidence suggested that the CRAG nomenclature could be applied to a grading system using only the macular centred field of the EURODIAB photographic protocol with no loss of sensitivity or specificity for the detection of referable retinopathy
In 2000, the National Screening Committee, through its Photographic Grading and Disease Management Working Party, produced a provisional alternative grading system to the EURODIAB grading system. There were minor differences with the CRAG grading system in language e.g. background retinopathy vs. non proliferative retinopathy, but more fundamental differences in terms of the number of grades defined and the requirement for any lesion counting- severity being assessed in comparison with standard photographs. There were also important differences with regard to maculopathy in that the main area of interest was less (circle of radius 0.5 DD vs. 1.0 DD), except where circinate exudates were present in which case the area of interest was substantially larger. Haemorrhages alone in the macula were disregarded in the absence of a reduction in visual acuity.
The provisional NSC grading system produced in 2000, was pragmatic, based on consensus expert opinion, but did not have a rigorous outcome related evidence base, and had not been widely adopted in screening programmes elsewhere in England & Wales.
The table following compares the two systems, and is set out so that in each row there is rough equivalence. The provisional NSC system reduced the retinopathy grades to four based on the requirement to identify both any retinopathy and sight threatening retinopathy. In this model R0 and R1 did not require referral whilst R2 and R3 required referral and urgent referral respectively. In the CRAG system R2 was divided into three categories of BDR (moderate, severe and very severe), which might allow the option for a reduced screening interval for the BDR moderate group as opposed to referral. The NSC system included advanced diabetic eye disease with proliferative retinopathy on the basis that both would necessitate urgent referral. The definition of diabetic maculopathy was quite different in the two systems, with a three-step process and an effectively twice as large area of potential interest in the NSC system.
The HTBS Topic Specific Advice group felt there might be advantage in recording the presence or absence of specific lesions within the reporting software. This would then allow the derivation of a summary grade through the application of a rule-based algorithm.
In view of the above points, a modification of the CRAG grading system was recommended in Scotland for screening for diabetic retinopathy.
Comparison of CRAG and Provisional NSC 2000 Grading Systems:
|
CRAG |
NSC |
||
| 1 | No diabetic retinopathy anywhere |
R0 |
No diabetic retinopathy |
| 2 | Background diabetic retinopathy (BDR) – mild
|
R1 |
Background diabetic retinopathy
|
| 3 | BDR – moderate
Any one of the following:
|
R2 |
Pre-proliferative diabetic retinopathy
Any of the following:
Cotton wool spots are not diagnostic of R2, but should promote a careful |
| 4 | BDR – severe
Any one of the following:
|
||
| 5 | BDR – very severe
|
||
| 6 | Proliferative diabetic retinopathy (PDR)
|
R3 |
Proliferative diabetic retinopathy
Any of the following features:
|
| 7 | PDR – High risk
|
||
| 8 | Advanced diabetic eye disease
Any of the following:
|
||
| 9 | Enucleated eye | ||
| 10 | Not adequately visualised
|
U |
Ungradeable
Images ungradeable due to any of
|
| Macula
11 |
Diabetic maculopathy present
|
M |
|
|
P |
Photocoagulation
|
||
|
OL |
Other lesions
|
The initial modifications comprised:
- disregard of cotton wool spots in isolation, as these lesions have no greater
prognostic significance than hard exudates (ETDRS trial) - addition of a separate record for laser photocoagulation burns and other
significant non diabetes related coincidental lesions - an alteration to the grading rules for single field photography to guarantee
no possibility of under grading retinopathy at any break point.
ORIGINAL SCOTTISH DIABETIC RETINOPATHY GRADING SYSTEM
|
Grade |
Single macular field photography |
Two-field photography or slit lamp |
| 1 | No diabetic retinopathy anywhere | No diabetic retinopathy anywhere |
| 2 | Background diabetic retinopathy (BDR) – mild
|
Background diabetic retinopathy (BDR) – mild
|
| 3 | BDR – moderate
(Inferior and superior hemi-fields delineated by a line passing through |
BDR – moderate
Any one of the following:
(Quadrants defined by two perpendicular lines intersecting at the centre |
| 4 | BDR – severe
Any one of the following:
|
BDR – severe
Any one of the following:
|
| 5 | BDR – very severe
|
BDR – very severe
|
| 6 | Proliferative diabetic retinopathy (PDR) – early
|
Proliferative diabetic retinopathy (PDR) – early
|
| 7 | PDR – high risk
|
PDR – high risk
|
| 8 | Advanced diabetic eye disease
Any of the following:
|
Advanced diabetic eye disease
Any of the following:
|
| 9 | Enucleated eye | Enucleated eye |
| 10 | Not adequately visualised
|
Not adequately visualised
|
| Macula
M1 |
Diabetic maculopathy early
|
Diabetic maculopathy early
|
| Macula
M2 |
Diabetic maculopathy observable
|
Diabetic maculopathy observable
|
| Macula
M3 |
Diabetic maculopathy referable
|
Diabetic maculopathy referable
|
| Photo-coagulation | Laser photocoagulation scars present | Laser photocoagulation scars present |
| Other | Other non-diabetic lesion present
|
Other non-diabetic lesion present
|
REASONS FOR SDRGS 2003
In late 2002 it became clear that it would make sense to try and unify all the current UK grading schemes. It also became apparent that not all screening programmes in Scotland were planning to use grading software. At the same time the American Academy of Ophthalmologists published a modification of the ETDRS grading system, that reinforced the approach of the HTBS, whilst also simplifying the process. This simplification did not change the referral criteria but made grading simpler by collapsing severe and very severe background retinopathy together and collapsing early proliferative and high-risk proliferative retinopathy together. These changes were encorporated into SDRGS 2003 bringing the Scottish grading system closer to the simpler system provisionally proposed for England.
Finally an important paper by George Bresnick, published in Ophthalmology 2000, emerged which enabled the maculopathy grading criteria to be safely refined. This paper showed that the presence of any hard exudates within a one disc-diameter radius of the centre of the retina had an extremely high sensitivity of 94% for detecting the presence of clinically significant macular oedema (specificity 54%). It was therefore felt that haemorrhages/microaneurysms could be safely dropped from the referable criteria for maculopathy. Blot haemorrhages were retained as it is not yet clear exactly why one-field screening is as effective as two-field. It was felt that blot haemorrhages might be a surrogate marker for referable retinopathy outside the disc-macular field of one-field screening. Also blot haemorrhages might be a surrogate marker for ischaemic maculopathy, a condition that requires special attention to glycaemic control and blood pressure control if progression is to be ameliorated.
