2 The Scottish Diabetic Retinopathy Grading System
Seven-field stereoscopic photography is a diagnostic technique that is not really suited to screening. The Scottish Diabetic Retinopathy Grading system has simplified the “4-2-1” rule of the ETDRS (see later) and applied it to a one-field non-stereoscopic grading protocol. A standard grading nomenclature for screening diabetic retinopathy is essential for consistent grading, for internal and external quality assurance purposes, for ease of exchange of data between clinical information systems, and for agreement on referral thresholds. A grading system needs to be of sufficient complexity to enable triage of patients into appropriate clinical outcomes e.g. referral to ophthalmology, routine re-screen, re-screen at reduced interval, but should not be unnecessarily complex. The important break points are the presence of any diabetic retinopathy and the presence of referable or potentially sight threatening diabetic retinopathy. The latter category may include the presence of lesions within the vicinity of the macula.
The Scottish Diabetic Retinopathy Grading System 2003 is a simplified version of the original grading system recommended by HTBS. It is almost identical to the American Academy of Ophthalmology “International Clinical Disease System for Diabetic Retinopathy”. The main difference is that the American system is designed for ophthalmologists using slit-lamp biomicroscopy rather than for screening programmes using non-ophthalmologists and digital photography. It is hoped that SDRGS 2003 will allow easy exchange of data with the evolving English grading system being developed on behalf of the National Screening Committee, as well as those grading systems proposed for Wales and Northern Ireland.
SCOTTISH DIABETIC RETINOPATHY GRADING SYSTEM 2003
Retinopathy
|
Retinopathy |
Description |
Outcome |
| R0 | No diabetic retinopathy anywhere | Rescreen 12 months |
| R1(mild) | Background diabetic retinopathy BDR – mild
|
Rescreen 12 months |
| R2(moderate) | BDR – moderate
(Inferior and superior hemi-fields delineated by a line passing through the centre of the fovea and optic disc) |
Rescreen 6 months(or refer to ophthalmology if this is not feasible) |
| R3(severe) | BDR – severe Any of the following features:
|
Refer ophthalmology |
| R4(proliferative) | Proliferative diabetic retinopathy PDR Any of the following features:
|
Refer ophthalmology |
| R5(enucleated) | Enucleated eye | Rescreen 12 months (other eye) |
| R6 (inadequate) | Not adequately visualised
|
Technical failure. Arrange alternative screening examination |
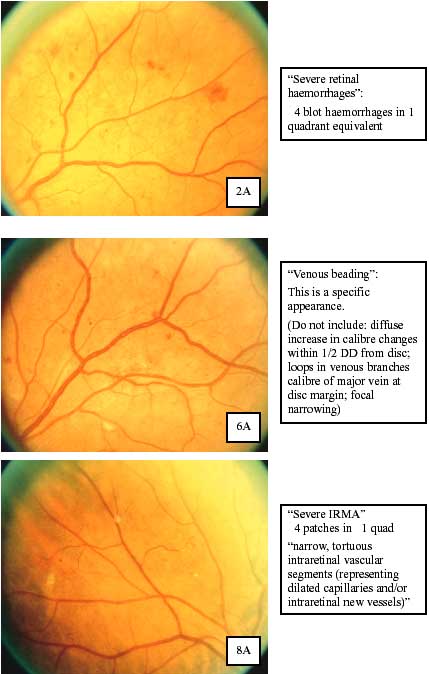
- Severe retinal haemorrhages >= Airlie House slide 2A (“4 blot haemorrhages”)
- IRMA >= Airlie House slide 8A >=4 patches in >=1 quad “Narrow, tortuous intraretinal vascular segments (representing dilated capillaries and/or intraretinal new vessels)”
- VB >= Airlie House slide 6A.Venous Beading. Diffuse increase in calibre is not included. Ignore changes within 1/2 DD from disc.
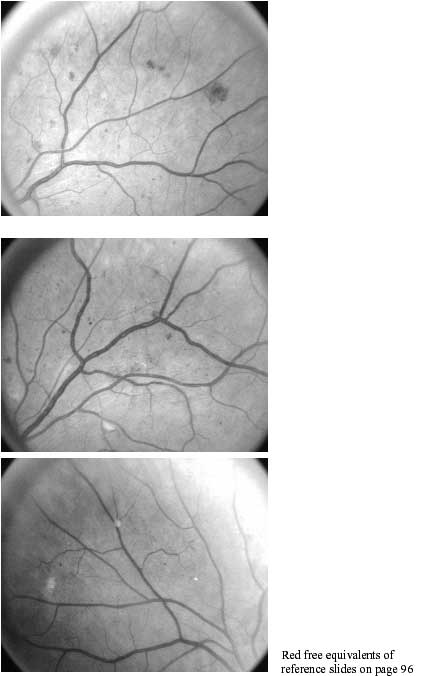
The Airlie House standard photographs are freely available at http://eyephoto.ophth.wisc.edu/ResearchAreas/Diabetes/DiabStds.htm
Other venous abnormalities do not constitute venous beading and their presence is of uncertain significance:
- loops in venous branches
- definite focal narrowing
Maculopathy
Diabetic maculopathy is a confusing term. Strictly speaking maculopathy refers to retinopathy affecting the macula. Clinicians in the UK also use this term interchangeably with the term “diabetic macular oedema”. In a screening context macular oedema or retinal thickness often cannot be visualised with the screening technology being utilised. Therefore surrogate markers such as haemorrhage and exudate at the macula are used to identify patients at risk of having or developing macular oedema. In SDRGS the term diabetic maculopathy will be used to indicate “retinopathy at the macula requiring referral to an ophthalmologist to confirm or refute the presence of diabetic macular oedema”.
|
Maculopathy |
Description |
Outcome |
| M1 (Observable) | Lesions within a radius of > 1 but – 2 disc diameters of the centre of the fovea
|
Rescreen 6 months (or refer to ophthalmology if this is not feasible) |
| M2 (Referable) | Lesions within a radius of – 1 disc diameter of the centre of the fovea
|
Refer ophthalmology |
Other Features
|
Coincidental findings |
Description |
Outcome |
| Photo-coagulation |
|
No Action |
| Other | Other non-diabetic lesion present
|
As clinically indicated |
Referable Retinopathy
Referable retinopathy comprises any of:
- BDR of grade moderate or worse (R2)
- PDR (R4)
- Diabetic maculopathy observable (M1)
- Diabetic maculopathy referable (M2)
However, patients graded BDR moderate (R2) or diabetic maculopathy observable (M1), in the absence of other features of referable retinopathy need not necessarily be referred to an ophthalmologist, as laser therapy would not be indicated immediately. However, this policy should only be followed if arrangements can be made to re-screen these groups at six monthly intervals. In the absence of a facility to offer re-screening at a six-month interval all patients whose worst eye is graded, as BDR moderate (R2) or diabetic maculopathy observable (M1) should be referred to an ophthalmologist.