4 Ophthalmic Classification
As seven-field photography is not a practical every day tool for ophthalmologists or other clinicians, the ETDRS presented the following grading scheme at the “Diabetes 2000” symposium of the 1991 annual meeting of the American Academy of Ophthalmology. This divided up retinopathy into non-proliferative and proliferative diabetic retinopathy. A separate category was described for retinal thickening involving the centre of the retina- the area known as the macula, which is responsible for central vision. This latter category was termed diabetic macular oedema.
NON-PROLIFERATIVE RETINOPATHY
This is graded into one of four categories, which predict the likelihood of progressing to proliferative retinopathy. In particular the 4-2-1 rules were developed to define severe and very severe diabetic retinopathy.
The 4-2-1 Classification Of Diabetic Retinopathy.
|
Classification |
Features |
| Mild | >1 microaneurysm |
| Moderate | Severe retinal haemorrhages in 1-3 quadrants, or venous beading or IRMA definitely present. |
| Severe | Any one of: 4 quadrants of severe retinal haemorrhages, 2 quadrants of venous beading, 1 quadrant of moderately-severe IRMA |
| Very Severe | Any two of the severe features |
The whole purpose of this classification is to attempt to predict the likelihood of progression to proliferative diabetic retinopathy and thus indicate safe screening intervals for patients and clinicians. As can be seen from the following graph there appears to be an almost linear increase in the risk of developing proliferative retinopathy with each step up the severity scale.
|
Classification |
Screening Intervals |
| Mild |
12 months |
| Moderate |
6 months |
| Severe |
3-4 months |
| Very Severe |
2-3 months |
Using this classification the American Academy of Ophthalmology recommended the following screening intervals for non-proliferative diabetic retinopathy.
PROLIFERATIVE RETINOPATHY
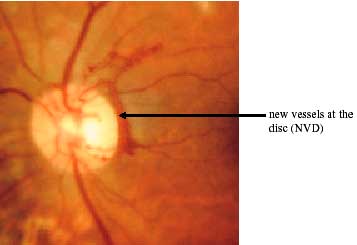
Proliferative retinopathy is defined by the presence of new vessels. These were defined by their location as being either present at the disc or within one disc diameter of the disc (NVD) or elsewhere (NVE). The distinction is important as the presence of NVD signifies a far greater risk of visual loss than NVE.
Proliferative retinopathy was categorized into early proliferative diabetic retinopathy or high-risk proliferative diabetic retinopathy. To be categorized as having high-risk proliferative diabetic retinopathy three of the following four features had to be present:
1. Presence of new vessels.
2. Location of new vessels on or within one disc diameter of the optic disc (NVD).
3. Severity of new vessels-
NVD equal or greater than one-fourth to one-third disc area
NVE equal or greater than one-half disc area
4. Vitreous or pre-retinal haemorrhage.
DIABETIC MACULAR OEDEMA
Diabetic macular oedema was defined as the appearance of retinal thickening at the macula caused by the presence of fluid outside cells (extracellular oedema) or inside cells (intracellular oedema). Diabetic macular oedema is categorized into:
- Circinate
- Diffuse
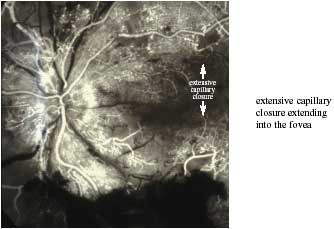
- Ischaemic
- Mixed
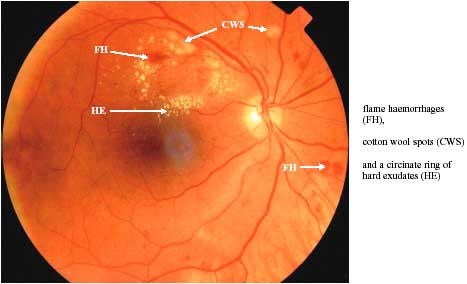
Circinate macular oedema refers to the presence of focal areas of macular oedema (retinal thickening) with surrounding hard exudate formation and is the result of focal leakage.
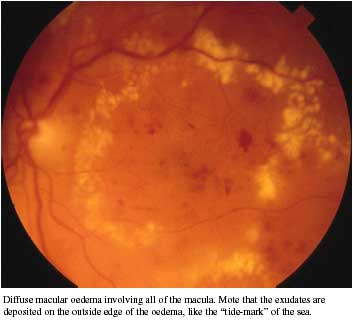
Ischaemic macular oedema can only be identified by fluorescein angiography. Many patients have a combination of all three categories and are categorized as having mixed macular oedema