Artery occlusion
Retinal arteries are end arteries and are therefore prone to occlusion by emboli. Like retinal veins they may also occlude as a result of vessel wall inflammation (usually giant cell arteritis) or as a result of an underlying clotting disorder (thrombophilia). Raised intraocular pressure can occlude the artery but only if the pressure is extremely high. This is only usually seen in patients with a severe attack of acute angle closure glaucoma.
BY EMBOLI
A common cause is an embolus originating anywhere from the heart to the ophthalmic artery.
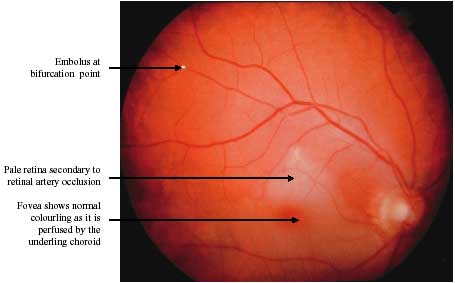
Common sites where emboli form are the aortic valve in the heart and the carotid artery in the neck. If the clot lodges in the blood supply to the back of the eye it will cause sudden loss of vision (amaurosis fugax).
Patients with a recent history of amaurosis fugax should be considered for carotid endarterectomy, as it may be a warning sign that the internal carotid artery is about to occlude which may result in a devastating stroke. A cardiac source should always be considered particularly if the patient has atrial fibrillation (an irregular pulse where the heart contracts ineffectively) or a murmur suggesting a problem with the heart valves. Patients in atrial fibrillation should usually be anticoagulated if they have had amaurosis fugax or a retinal artery occlusion. All other patients should be commenced on low dose.htmirin.
Asymptomatic patients who are found by chance to have emboli in their retinal arteries have not been shown to benefit from carotid endarterectomy. Until there is evidence to prove otherwise, they should not be offered surgery as there are significant risks of death or disability (8% of patients die or suffer a disabling stroke). They are, however, at increased risk of stroke and should receive the same medical management as those patients with symptomatic emboli.
Hypoperfusion
Atherosclerosis of the ophthalmic artery or of the internal carotid artery can lead to hypoperfusion of the whole eye. Such patients often present with blurred vision or pain. Blurred vision is a result of the very slow blood flow to the eye resulting in a lack of oxygen and vital nutrients being delivered to the eye. Examination of the retina may reveal little wrong or may show scattered haemorrhages, especially temporal to the macula. Often the diagnosis is only made by fluorescein angiography, which reveals the very slow flow of fluorescein through the retinal circulation. As well as the fundus the front of the eye (the anterior segment) can become ischaemic resulting in the growth of new vessels on the iris (rubeosis iridis or proliferative iridopathy). This is often associated with pain even if the pressure in the eye is not particularly raised.
Often such patients have severe carotid artery stenosis. Unfortunately, endarterectomy has not yet been shown to be beneficial in this situation, probably reflecting the fact that there may be widespread damage to the carotid artery tree. Such patients should be managed as noted above. If the eye is painful this often responds to topical dilation of the pupil with atropine and topical steroid drops. Unfortunately laser treatment is rarely helpful reflecting the fact that the whole blood supply is affected rather than just the capillary network of the retina.
OTHER UNRELATED DISORDERS
Ageing
Ageing has many effects on the eye. In the retina it can affect the retinal pigment epithelial layer. This layer is highly metabolically active. With age it appears to deal less with toxic by-products and starts to deposit featureless material under itself (drusen).
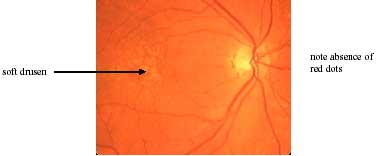
DRUSEN MACULOPATHY
Drusen in themselves do not affect vision. There are two main forms depending on the size.

If they are less than 64microns in diameter (half the width of a retinal vein at the disc) then they are termed hard drusen. If they are greater than 64 microns they are termed soft drusen. Soft drusen are more significant as they represent small detachments of the retinal pigment epithelium from its underlying basement membrane. Soft drusen can be a forerunner of atrophy or choroidal neovascular membrane formation.
Drusen therefore do not constitute age-related macular degeneration in themselves. They can usually be differentiated from hard exudates by the absence of any adjacent microaneurysm.
AGE-RELATED MACULAR DEGENERATION
There are two main forms of age-related macular degeneration:
- atrophic (dry) age-related macular degeneration
- neovascular (wet) age-related macular degeneration
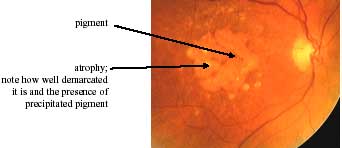
Atrophic Age-Related Macular Degeneration
In the atrophic form the retinal pigment cells die off. When they do so, they precipitate out any pigment they contain. Th1s leads to well demarcated pale areas with adjacent deposits of pigment. As the overlying photoreceptors no longer have the underlying retinal pigment cells they need to nourish them, they die too. This results in gradual visual impairment.