NEW VESSEL FORMATION
New blood vessels come from the endothelial cells of post-capillary venules. For these endothelial cells to form a new blood vessel several events have to occur.
The endothelial cell has to:
- become activated
- be released from its surroundings
- move (migrate)
- increase in number and form tubes (proliferate)
Endothelial Cell Activation
Endothelial cells become activated in response to growth factors released from the cells of the retina and the circulation. Ischaemic but not infarcted retina (i.e. just alive) appears to release local growth factors that activate endothelial cells in healthy capillaries at the edge of the ischaemic area. The most important growth factor is vascular endothelial growth factor (VEGF). VEGF is released by the retinal pigment epithelial cells in response to hypoxia. VEGF is also produced by the retinal pigment epithelial cells in response to hyperglycaemia through activation of the protein kinase C pathway. Other sources of growth factors include the platelets and white blood cells that occlude the capillaries. Indeed some of the adhesion molecules produced by endothelial cells, that cause white blood cells to stick to them, induce new vessel formation themselves.
Matrix Degradation
Endothelial cells sit on a basement membrane. Break down of this basement membrane and its surrounding structures must occur if the endothelial cells are to escape (migrate) and form new blood vessels. The cause of this is unknown. As a result the activated endothelial cells are exposed to various proteins such as laminin that provide a platform for the endothelial cells to grow on. Laminin, a major component of the basement membrane, appears to play a key role in the growth of retinal capillary endothelial cells. Degraded (“broken down”) laminin appears to stimulate angiogenesis whereas intact laminin appears to have the opposite effect. Breakdown of collagen also has to occur. Basement membranes appear to have particularly high levels of type IV collagen, which appears to inhibit angiogenesis and presumably must also be degraded if angiogenesis is to occur.
Endothelial Cell Migration And Proliferation
Once the endothelial cells have become activated and the basement membrane has been degraded the endothelial cells then migrate from the post-capillary venules into the surrounding tissue (matrix). As they migrate, more cells and tubes are formed. Pairs of tubes join together thus forming loops. The top of the loop then forms further tubes that go through the same process producing further loops. This process is controlled by growth factors such as urokinase type plasminogen activator (µPA) and transforming growth factor beta (TGF beta). In response to VEGF, µPA stimulates cells to migrate whereas TGF beta is responsible for maturing the proliferated cells into capillary tubes.
Clinical Appearance of New Vessels

New vessels grow from the walls of post-capillary venules. Clinically, they therefore appear to be growing from veins and not from arteries. They always form loops. In this respect they disobey the law of fractals. Fractals are a geometrical pattern whose parts resemble the whole. This is often seen in nature with for example trees. Trees, like, blood vessels, have a central trunk that then divides into smaller branches which then divides into smaller twigs. Each component looks similar. New blood vessels do not divide into smaller and smaller components. Indeed their diameter is often bigger than the vessel they originated from, and instead of dividing into smaller components they loop back to their
originating vessel.
The commonest site where confusion may arise as to whether a new vessels is present or not is at the optic disc. Here there are often small vessels radiating out from the disc. New vessels growing from the optic disc are the ones most likely to bleed so there is always concern that a small blood vessel rising from the disc may be a new blood vessel. Normal small blood vessels, however, always taper to an end and do not loop back to the disc. New vessels, however, always loop back and the top of the loop often has a wider diameter than the start of the loop.
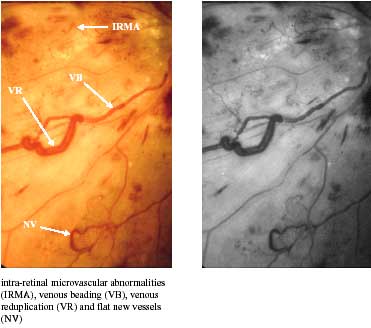
New blood vessels are often confused with IRMA. As explained earlier, formation of IRMA occurs within areas of capillary occlusion whereas new vessels occur along the border between healthy retina and areas of capillary occlusion. Although IRMA do not always obey the laws of fractals, they never form loops. Any unusual blood vessel that may be forming loops should always be considered as a new vessel until proven otherwise.
NEW VESSEL BLEEDING

New blood vessels do not grow within the layers of the retina but between the inner surface of the retina and the vitreous gel.

Indeed new blood vessels grow into the vitreous gel itself along its posterior (back) hyaloid surface. The growth of the new blood vessel into the gel results in an inflammatory response and scar formation. This scar formation is initially transparent. As scars always contract the gel appears to pull away from the new blood vessel. This results in either the new blood vessel being pulled forward and appearing to stand up or in the blood vessel tearing and bleeding or a combination of both.
